

Hannah McCabe, RN in the Adult ICU at VGH, reviews vital signs in the EHR that are uploaded from a vital signs monitor (VSM) shown in the background at her patient's bedside.
As the IHealth team and partners continue to roll out advanced functions of the electronic health record (EHR) across the region, we looked at 11 ways this multi-year project contributes to safer, quality patient care and a better experience for care teams.
1. Barcode scanning of medications and patient armbands
At sites that have activated CPOE (computerized provider order entry), nurses use a barcode scanner to verify both the patient's armband identification and the medication label. This process ensures that the correct medication is administered to the right patient, as ordered. Barcode scanning reinforces adherence to the 10 "rights" of medication administration, enhancing accuracy and patient safety with every dose.
2. Reduced duplication of diagnostic tests and lab work
When a patient's detailed health record is visible in the EHR by different care team members, no matter their location in Island Health, this helps prevent duplicated or unnecessary diagnostic tests and lab work. When a patient presents at their family doctor, a specialist appointment, or in the hospital, their detailed health information, including previous tests and lab results, is available electronically. That saves time for the patient and care team members and helps to streamline access to the busy departments providing the tests and imaging results.
3. FetaLink traces real-time heart beats
FetaLink displays real-time fetal heart rate tracings in the labouring patient's chart in the EHR. Replacing paper tracings, FetaLink gives immediate access to information that helps providers make critical and timely decisions for patients and their babies. Care for labouring patients is less intrusive, as providers and nurses can view the electronic data outside the room. VGH was the first Island Health site to implement FetaLink, going live with the new tech in September.
4. Standardized assessment with InterRAI-CA
InterRAI-CA is a new tool embedded in the EHR that standardizes community health services intake assessments and helps clinicians determine both what clients need and how urgently they need it. It's a big step forward in providing both individual patient and population health information to Island Health staff.
5. Tap N Go
The Tap N Go system now installed at many Island Health sites works with staff proximity access cards (prox cards) to help staff unlock computer screens and move between workstations faster than they could by typing in a username and password dozens of times a day. Tapping in to access their patients' information is quicker, then tapping out after each session ensures a patient's information remains private and protected.
6. eMOST
When a patient is unable to express their wishes in an emergency or urgent health situation, having eMOST (electronic medical orders for scope of treatment) in place ensures care team members can honour the patient's wishes for important care decisions. Patients who work with their provider to register an eMOST through Advance Care Planning have peace of mind that anywhere they seek care at Island Health acute care facilities, their eMost will be available to care providers.
7. MyHealth Patient Portal
The MyHealth patient portal connects patients and clients (or their proxies) via their own device to lab results, imaging reports and 58 different types of clinical notes from providers. With access to MyHealth, patients can take greater control of their health care journeys. Health care providers benefit from patients invested in and informed about their care. Enrolment in the MyHealth Patient Portal has surpassed 274,000 people.
8. Patient tracking boards in perioperative areas
Patient tracking boards in the perioperative area at NRGH, RJH, VGH and South Island Surgical Centre are described as a “game changer" for staff. The boards, which tell staff and care teams from admission through to recovery where each patient is in the surgical process, are also viewable in waiting rooms. There, waiting family members are issued a code to identify their family member, and use it to track their progress through perioperative stages.
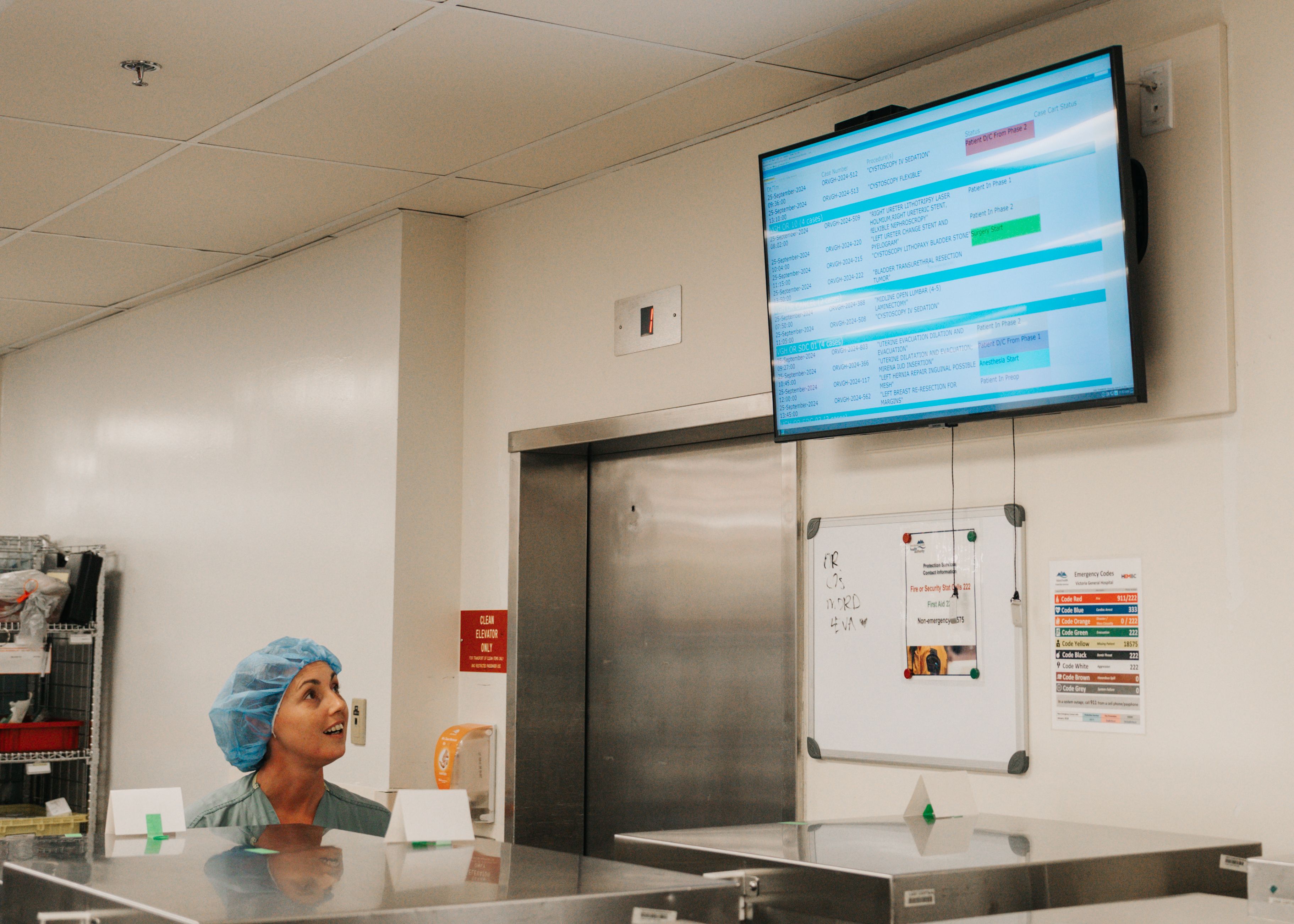
Alicia Bauln, an Assistant in the MDRD, views the new digital tracking board at VGH.
9. Communication and transfers in care
Patients transferring between facilities or back to the community now benefit when their information follows them in one electronic record. Vital information is available ahead of the patient's arrival, helping health care teams make the best decisions for their ongoing care. The receiving team has the patient's medication list and treatment history readily available, so the patient doesn't need to repeat these details.
10. Electronic order sets
Order sets, both electronic and on paper, are valuable decision support tools for providers that are grounded in both local and regional guidelines and standards for best practice. Transitioning order sets into the EHR involves subject matter experts, representing medical and clinical staff from across our region, who review existing order sets and develop new ones. Order set use reduces unnecessary variation in care. With the transition from paper to electronic order sets at CPOE-activated sites, quick access supports greater use of order sets by providers and efficiencies in care.
11. EHR-connected vital signs monitors
Vital signs monitors (VSMs) make patient data immediately available to caregivers anywhere a member of their care team has access to the EHR. Biomedical devices upload patient vital sign data directly into the EHR in real-time, including a patient's heart rate, blood pressure, oxygen saturation and respiratory rate. This information is then available as part of the patient's record to all health care providers caring for the patient to support decision making and care planning.
Learn more about the EHR and IHealth benefits for patients and care teams.