Membership Callout:
- Explore opportunities to join teams leading quality improvement
-
Point-of-care staff are in the best position to see opportunities to improve the quality of patient care. Island Health's evolving approach to quality improvement is creating new opportunities for staff and medical staff to influence the quality of care in local sites and community programs.
New committees are being formed to help enable quality improvement in acute sites and community services across all Island Health communities. Point-of-care staff and medical staff are invited to bring their valuable knowledge and perspectives to these new tables.
Review the information on this page to learn more about these committees, member roles and responsibilities and the application process. When you are ready, please use the link below to share your contact information and identify the committees that you are interested in joining.
Click here to access the membership survey.
Download this PDF for further information surrounding opportunities for point-of-care-staff, instructions and the member identification process.
What's New:
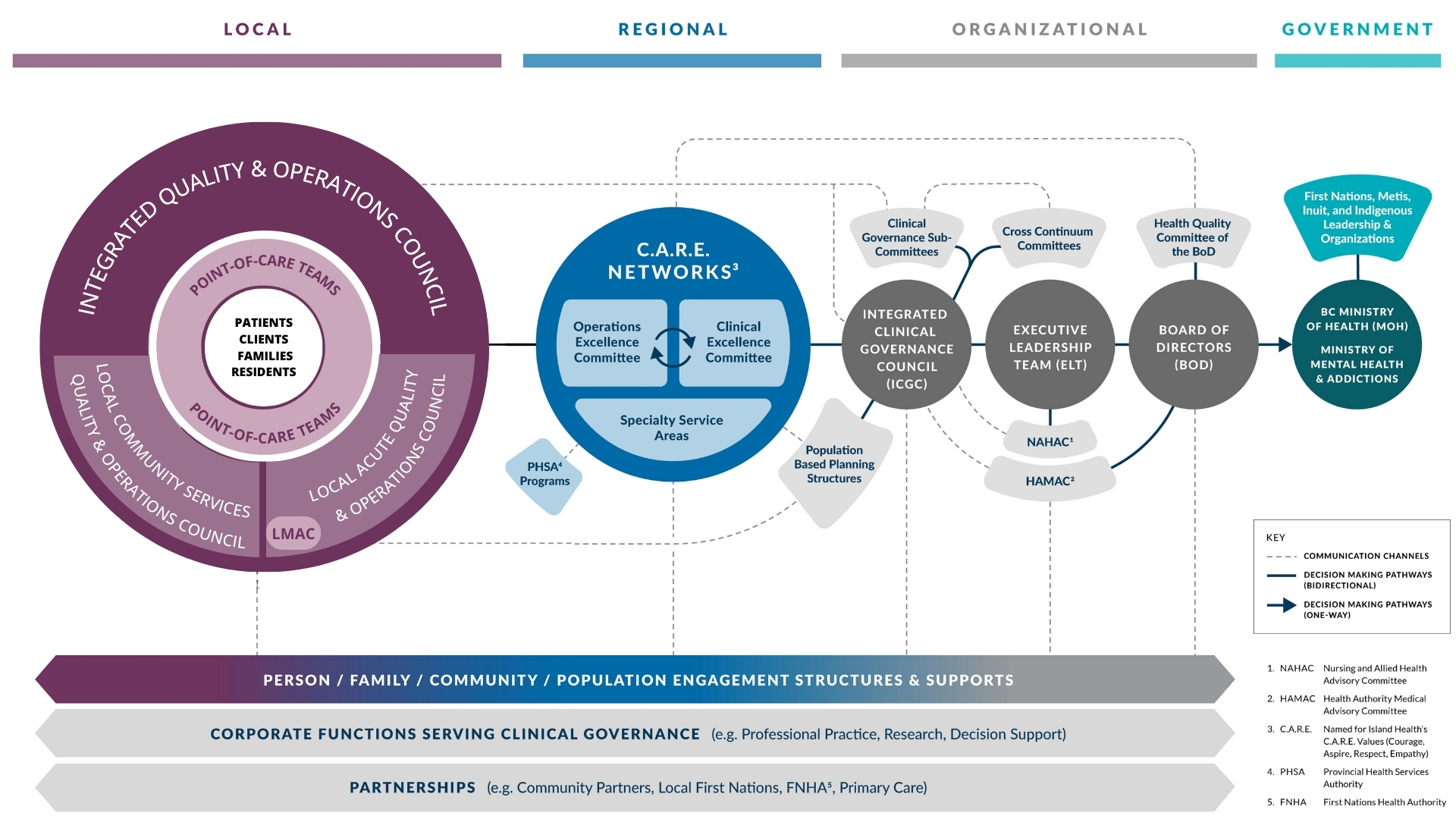
Updated Clinical Governance model
MILESTONE: New local-level structures complete
Island Health's clinical governance model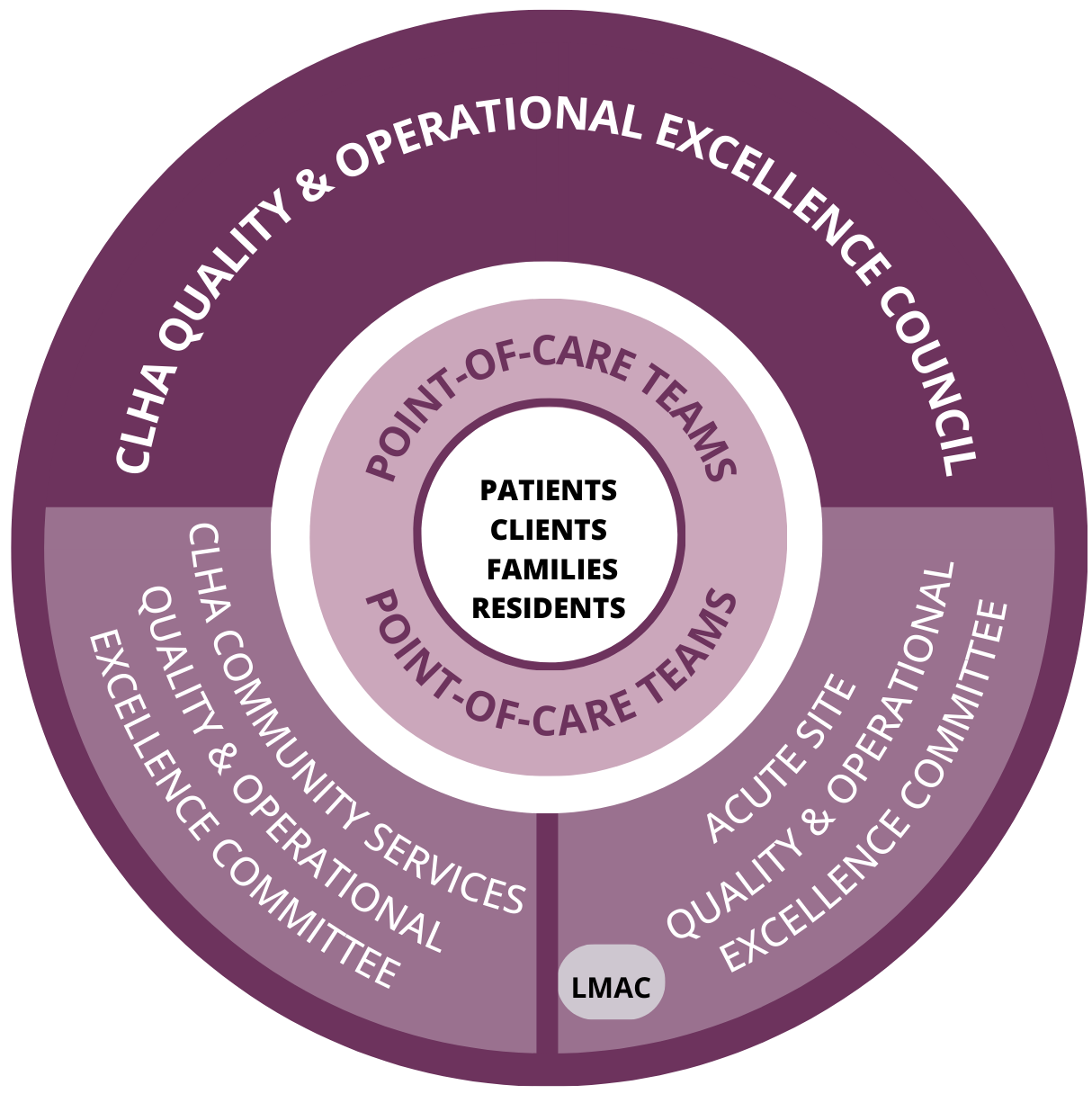
A new design for local clinical governance committees that brings together acute, community, medical and patient perspectives is now part of Island Health's modernized clinical governance structure. This achievement is an important milestone in Island Health's journey to strengthen and streamline the way we work together to make decisions about the quality and safety of patient care.
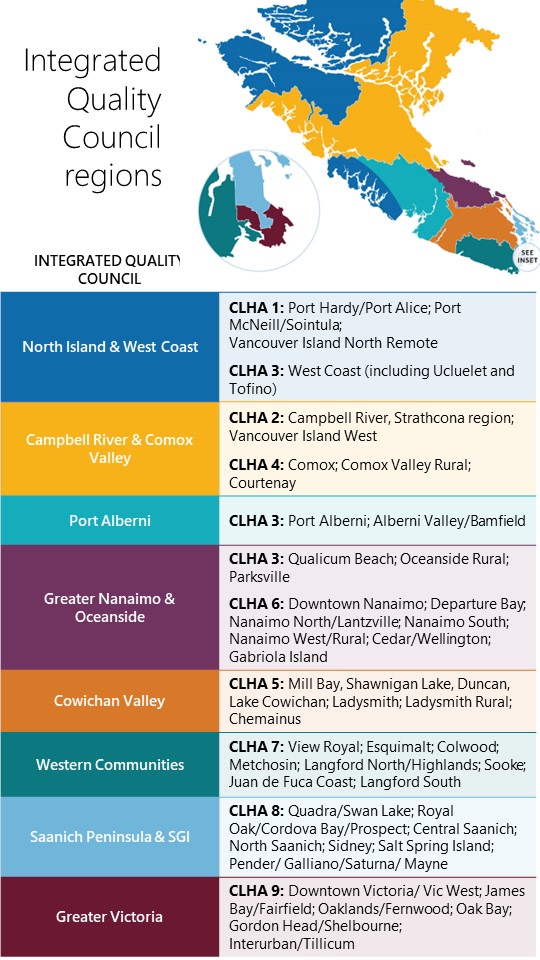
While regional C.A.R.E. Networks are focused on specific services, eg: Diagnostic Imaging or Critical Care, the local clinical governance committees will focus on services and sites within eight geographic regions. The committee structures, and their accountabilities and mandates, were developed collaboratively over the last six months. While designed to create consistency across Island Health, some regions may have fewer committees to reflect their unique geography and leadership structures.
Core committees include:
CLHA Quality & Operational Excellence Council: Forum for representatives from all site-based and community services to improve quality and outcomes across the continuum of care.
Acute Site Quality & Operational Excellence Committee: Site-based committees focused on optimal service delivery and operational efficiency within that site.
Community Services Quality and Operational Excellence Committee:
Integrated table for all community services (eg: Long-term care, Community Health Services) to focus on optimal service delivery and operational efficiency across community services.
The design was informed by Island Health's quality leaders and evidence-based best practices demonstrated by global leaders in clinical governance. The design will help create consistency between regions, and ensure that local committees have the resources, connections to other decision-making groups and clear decision-making rights to drive and influence change.
Leaders are working to identify core membership and advance detailed Terms of Reference for these committees, many of which will begin functioning this spring. Detailed membership principles, orientation and ways of working with other clinical governance committees, such as C.A.R.E. Networks, are actively in development.
FAST FACTS ABOUT NEW LOCAL CG STRUCTURES:
- Eight local areas have been identified (see map below), which align with Consolidated Local Health Area (CLHA) boundaries. Some boundaries have been modified to reflect patient flow and leadership structures.
- The model supports three core committees for each region: One focused on community-based services, one focused on acute sites and an integrated council that provides a forum for all sites and services.
- Aligning to this new design will necessitate the creation of 12 new committees and the adaption of 12 existing committees.
FEBRUARY NEWSLETTER: Look back at 12 months of progress and ahead to next steps on our journey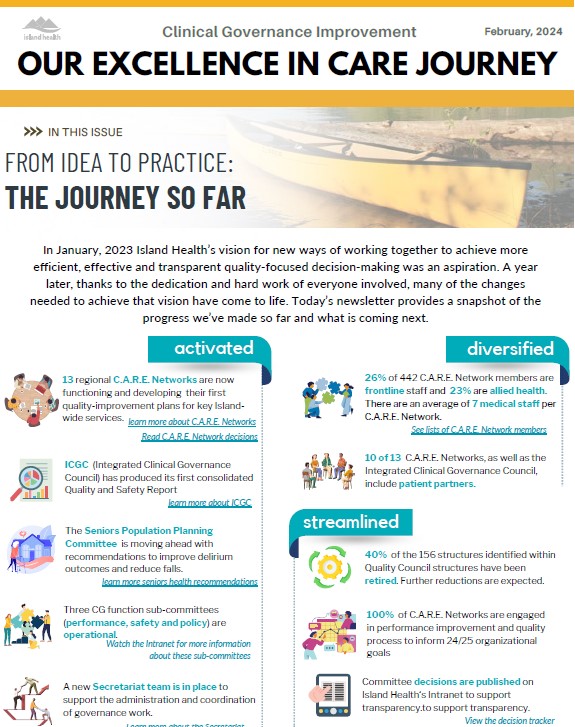
Feb. 20: A tremendous amount was accomplished in 2023 as we saw planned improvements to our clinical governance structures and processes move from idea to reality.
Check out this newsletter to read more about those successes and the work that will be accomplished this year, such as the implementation of local committees and development of a new Clinical Services Plan.
VIDEO: Snapshot of CGII progress
Nov. 20, 2023: Great progress is being made to strengthen Island Health's Clinical Governance - from C.A.R.E. Network decisions to designing local structures and activating key support structures. Check out this short video and watch this space for more details about your successes and information about what is coming in 2024.
OCTOBER NEWSLETTER: Meet the C.A.R.E. Network committee chairs, learn about new Office of the Secretariat supports and much more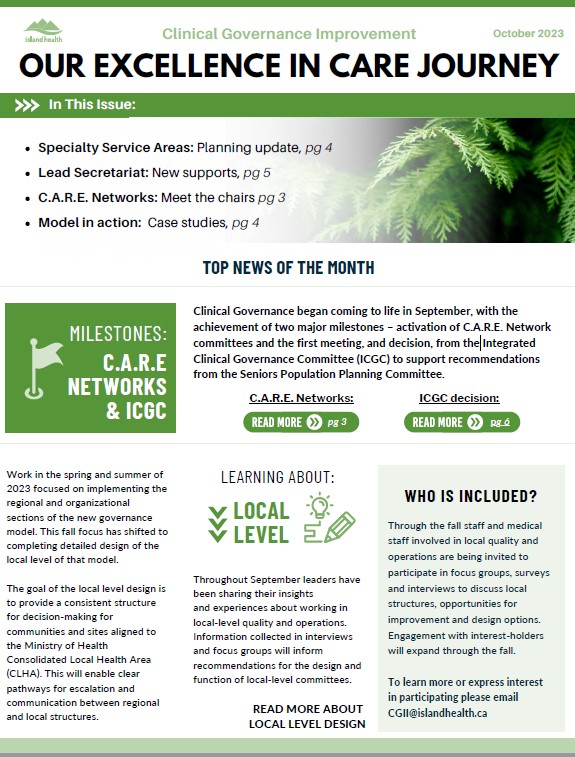
Oct. 10, 2023: The second edition of the CGII Newsletter includes a wealth of information and resources about clinical governance activities, including:
- The first meeting and decision from ICGC
- Scenarios to enhance understanding of the new governance model
- Designing the Speciality Service Area committees
- C.A.R.E. Network committee membership
We want your feedback! Please email CGII@islandhealth.ca and let us know what you would like to see in future issues.
Click here for the newsletter.
Meet your C.A.R.E. Network committee members
Oct. 4, 2023: C.A.R.E. Networks, which are replacing Quality Councils, became operational in September. Committees began meeting and working toward the development of their first annual quality plans. You can find the membership lists on the CGII Resource section of the Intranet.
VIDEO: Why should staff help lead quality improvement?
Point-of-care staff are in the best position to not only spot opportunities to improve the quality of patient care, but to understand how to successfully make those changes in a busy clinical environment. The question is, how can frontline experts bring those opportunities to light? One solution is to join a new clinical governance committee and become part of the team leading the future of quality improvement for Island Health. Continue reading
Learning from each other: Exploring the 'one canoe' model of care

Dec. 12, 2022 - At the recent Clinical Governance Change Summit we had the opportunity to share a conversation between Krista Allan, Island Health's Vice President for Knowledge and Practice and Chief Nursing Officer, and Connie Paul, a health-care leader and Nursing and Community Support Manager for Snuneymuxw Hulit Lelum, about collaboration, equity and change in health care.
Click here to watch the recording of their conversation.
|
According to the Health Standards Organization, clinical governance is the framework by which the governing body, leaders, and health care providers have responsibility and accountability for the quality of care. In the fall of 2021, in response to clear direction from our care teams, Island Health launched the Clinical Governance Improvement Initiative with the ultimate goal of improving clinical outcomes for patients and families. We continue to listen to our care teams and we are proud to be taking meaningful steps towards clear, simple, and transparent clinical governance and accountability. The CGII is a critical next step in strengthening our organizational foundation for culturally-safe high-quality care, and for helping us achieve our strategic framework goals by 2025. Questions?
FAQLooking for a report or document? Check out the Resources page. If you can't find what you're looking for please email CGII@IslandHealth.ca. |
Questions Inbox & Communication Resources
Do you have questions about the Clinical Governance Improvement Initiative or want to get more involved?
Send your request to CGII@IslandHealth.ca
.png)