Posted on: January 17, 2023
A man complaining of a sore, swollen arm seeks care at Chemainus Health Care Centre (CHCC) urgent care clinic and is diagnosed with an infection. The physician does a swab of an abscess on his arm and sends it for a culture test to determine antibiotic resistance.
The patient is started with a dose of IV antibiotics and asked to continue on oral antibiotics treatment, with instructions that his treatment be reviewed three days later by a second physician. The second physician sees the patient and notes that the infection is not improving.
As the culture test results are not yet available, the second physician changes the prescribed oral antibiotic to one that provides greater bacterial coverage.
Meanwhile, the man's family physician, Dr. Tanis Morris, receives copies of the culture test results at her practice. Looking through her patient's electronic file, she determines that the antibiotics prescribed will not kill the bacteria. She calls the patient and gets the oral and IV medication stopped before ordering a new prescription for her patient.
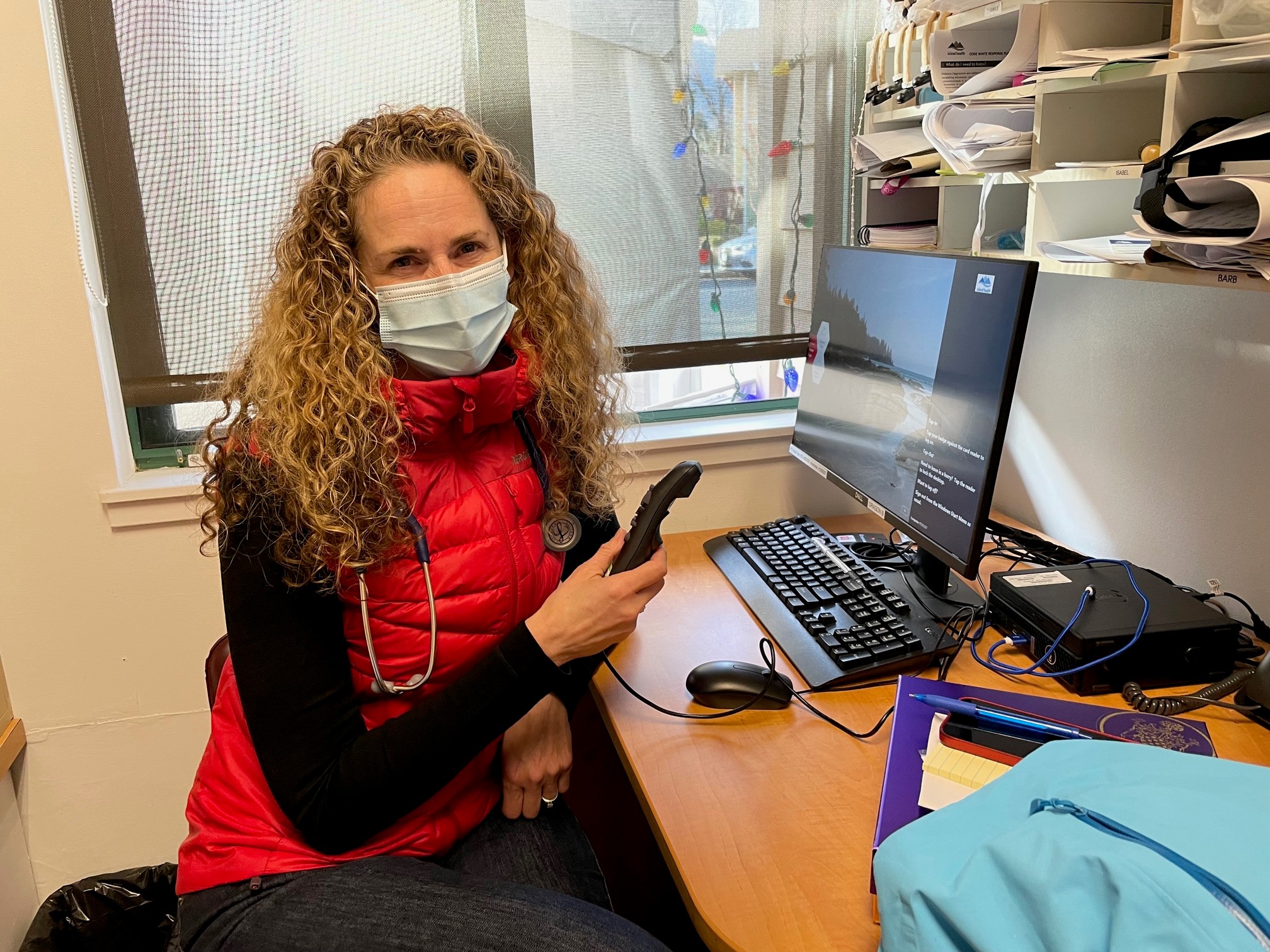
As Medical Lead at CHCC, Dr. Tanis Morris looks forward to the benefits to patients and care providers that come with electronic clinical documentation.
“It was only because the urgent care centre had just switched to FirstNet, with electronic documentation on my patient immediately available to me, that I became aware of my patient's visit to urgent care," says Dr. Morris. “I was able to see impressions from both physicians, and copies of the results from the swab, so I could intervene and help get his medication changed.
"In the past, that probably would have been a missed opportunity," she adds, with results from patients' tests often taking up to a week to arrive by mail. “I knew exactly from reading the first couple sentences what the plan was."
Access to patient records in EHR a “game changer"
Dr. Morris believes access to detailed clinical information on patients in the EHR is a “game changer" for physicians working in Island Health facilities and collaborating with colleagues in primary care clinics.
“Everything is there, it's clear, it's concise and it's readable. And that's what patients expect," she says.
Dr. Morris, as it happens, is also Medical Lead for CHCC urgent care alongside her family practice duties and was part of the IHealth “go-live" for electronic clinical documentation at CHCC in December.
The clinic team embraced the change, she said, including RNs Barb Leach and Laurie Schmidt, who completed their training early so they could help other staff get used to the new system.
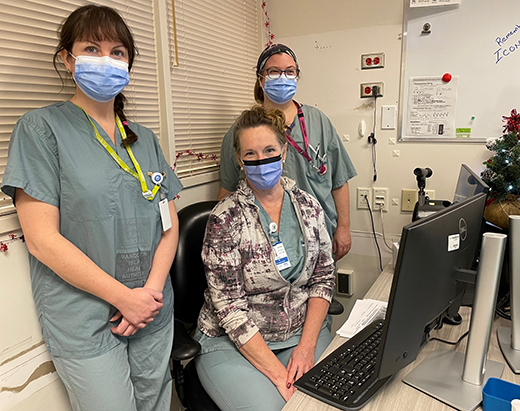
From left, RNs Erin McCoy, Laurie Schmidt and Liz MacLeod are getting more comfortable with electronic clinical documentation at CHCC in the weeks since go-live on December 6.
Schmidt has worked at CHCC for 18 years, 15 of those in urgent care.
While she considers herself “old school", as one of many nurses and other staff used to working with handwritten paper forms, she immediately saw the value of changing to electronic documentation.
“The doctors can right away see what's been charted on the patient," she says. “Before there was a lag time before the doctors' offices got the paper, and then they weren't very legible sometimes. So I can see that being a big value for the patient, and for the family doctors going forward."
Dr. Gary Toth, an emergency room physician at Cowichan District Hospital, is at CHCC today to take on a six-hour shift in urgent care. As he takes a few minutes at the computer to document, he recalls how arduous it was to document by hand, and welcomed the switch when CDH transitioned to ClinDoc in late September.
Dr. Toth was fully trained in ClinDoc when he recently started to help out at CHCC. “I'm so used to it, so it's been a very easy transition."
RN Erin McCoy, on staff at CHCC urgent care permanently since the summer, says she hopes that having ClinDoc activated may make it easier to attract physicians needed to staff the clinic.
McCoy and the CHCC team have welcomed doctors from CDH, Nanaimo Regional General Hospital, and the tertiary care sites in Victoria, who have taken on shifts -- allowing the clinic to stay open.
“They're used to the online charting. So it will be easier for them to just get into it and use FirstNet -- that's what they're used to," she says. “Overall it will be better. Especially if people have complicated histories."
Dr. Morris says the change to electronic clinical documentation comes at a critical time for CHCC urgent care, which has seen the volume of daily patients expand significantly compared to pre-COVID, while facing the challenge of recruiting new doctors.
Chemainus is similar to Oceanside and Ladysmith urgent care clinics, and continues to seek physicians trained to work in emergency medicine for temporary and permanent shifts.
Dr. Morris points to a pair of colleagues in her primary care practice as examples of new, young physicians who come with the expectation that electronic clinical documentation is part of their work when they take shifts in the urgent care clinic.
“They were already trained in (electronic clinical documentation), with tremendous experience using PowerChart over at St. Paul's (in Vancouver), and FirstNet," she says.
The possibility of attracting more medical students and new grads to work in primary care and to take shifts in urgent care, will hopefully increase now that ClinDoc has been implemented, she adds.
“We have to look at how our younger generation is being trained. We could stick with the paper and the quill and the chisel and the stone, because that's how we've always done things, but we have to remember that because we're not going to be here forever, we want to create a system that keeps moving even when we're gone."